How FIRAPY Improves Vascular Access for Hemodialysis
Vascular Access is a lifeline of ESRD patient
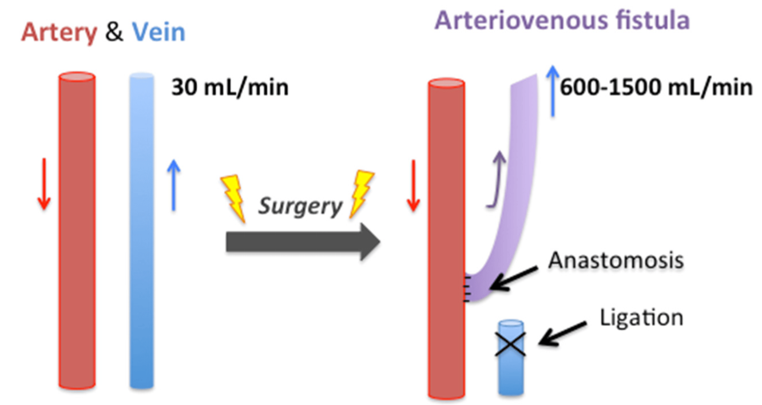
Vascular access is the lifeline for end-stage renal disease (ESRD) patients, enabling life-sustaining hemodialysis treatment. Ensuring the health and functionality of the arteriovenous fistula (AVF) or graft (AVG) is critical for effective dialysis, patient survival, and quality of life.
The Lifeline Fistula Won’t Last Forever—Here’s Why...
Luckly, we have FIRAPY.....
Increase the success rate of fistula maturation
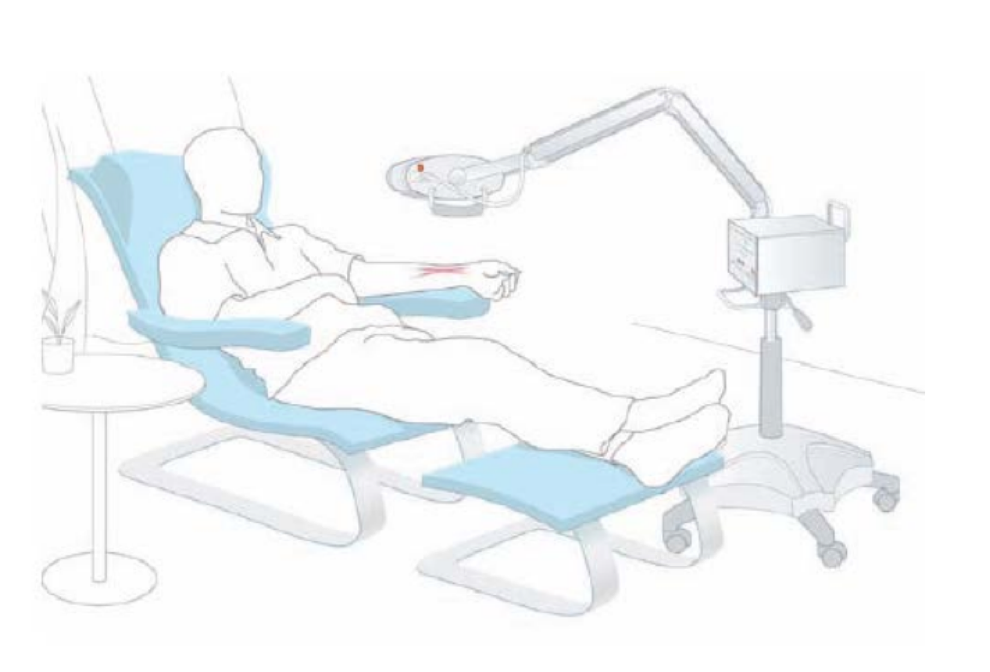
The one-month period after fistula procedure is the critical period for fistula maturation. FIRAPY (WS™ Far-infrared Therapy Unit) shortens maturation time, increases the fistula maturation success rate, improves fistula blood flow, and reduces the risk of fistula-related complications and the proportion of fistula failure.
Prolongs the life-span of the fistula
Human clinical trials have proven that long-term use of FIRAPY (WS™ Far-infrared Therapy Unit) extends the life-span of the fistula, decrease venous pressure, improves fistula blood flow, promotes circulation, prevents thrombosis formation, and reduces the number of surgeries required.
Improve Inadequate Blood Flow During Dialysis
FIRAPY (WS™ Far-infrared Therapy Unit) helps improve insufficient blood flow during hemodialysis by:
- Enhancing vasodilation and improving microcirculation
- Improving endothelial function and decreasing vascular resistance
- Alleviating localized inflammation and preventing complications that hinder blood flow
This makes FIRAPY a valuable adjunct in maintaining efficient and effective dialysis.
Reduces Cannulation Pain
Applying FIRAPY to the access area helps relieve pain during needle insertion by improving local circulation and relaxing surrounding tissues. It reduces sensitivity in the puncture zone, alleviates anxiety associated with repeated cannulation, and improves the overall experience for hemodialysis patients. The therapy is non-invasive, easy to use, and supports better tolerance to regular treatments.
Extends Time Between PTA Procedures
FIRAPY helps stabilize vascular access by improving endothelial health and reducing neointimal hyperplasia, one of the leading causes of access stenosis. By maintaining better blood flow and lowering the risk of restenosis, FIRAPY has been shown to prolong the interval between PTA procedures, reducing the need for frequent interventions and improving overall vascular access longevity for dialysis patients.
Clinical Experience from HD Staff

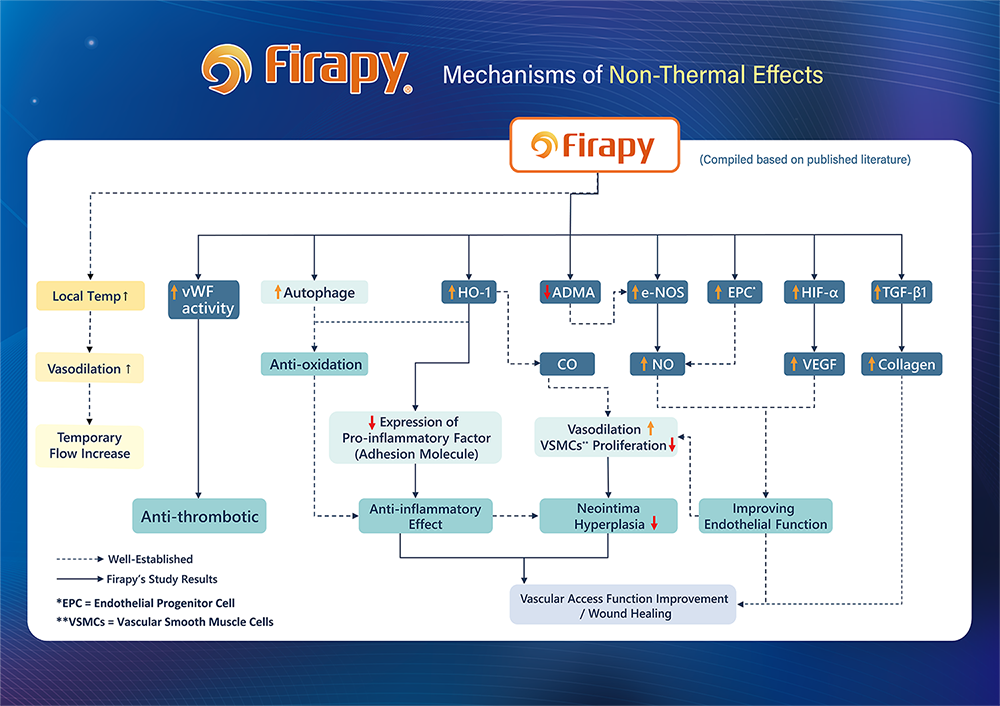
FIRAPY’s Non-Thermal Mechanisms in Vascular Applications
Reference:
- Lin, C. C., and et al. (2008). Far infrared therapy inhibits vascular endothelial inflammation via the induction of heme oxygenase-1. Arteriosclerosis, Thrombosis, and Vascular Biology
- Lin, C. C., and et al. (2022). Far-Infrared Therapy Improves Arteriovenous Fistula Patency and Decreases Plasma Asymmetric Dimethylarginine in Patients with Advanced Diabetic Kidney Disease: A Prospective Randomized Controlled Trial. Journal of Clinical Medicine
- Hsu, Y. H., and et al. (2012). Far-infrared therapy induces the nuclear translocation of PLZF which inhibits VEGF-induced proliferation in human umbilical vein endothelial cells. PloS one
- Hsu, Y. H., and et al. (2016). Far-infrared promotes burn wound healing by suppressing NLRP3 inflammasome caused by enhanced autophagy. Journal of Molecular Medicine
- Wu, C. W. and et al. (2006). Biological effect of far‐infrared therapy on increasing skin microcirculation in rats. Photodermatology, photoimmunology & photomedicine
- Huang, P. H., and et al. (2012). Far infra-red therapy promotes ischemia-induced angiogenesis in diabetic mice and restores high glucose-suppressed endothelial progenitor cell functions. Cardiovascular diabetology
- Chang, J. C., and et al. (2016). Far-infrared radiation protects viability in a cell model of Spinocerebellar Ataxia by preventing polyQ protein accumulation and improving mitochondrial function. Scientific reports
- Tu, Y. P., and et al. (2013). Postconditioning with far-infrared irradiation increases heme oxygenase-1 expression and protects against ischemia/reperfusion injury in rat testis. Life sciences
- Chen, C. H., and et al. (2022). Far‐infrared radiation alleviates cisplatin‐induced vascular damage and impaired circulation via activation of HIF‐1α. Cancer Science
- Chiu, H. W., and et al. (2017). Far-infrared suppresses skin photoaging in ultraviolet B-exposed fibroblasts and hairless mice. PLoS One